Abstract
Introduction: Chronic granulomatous disease (CGD) is a primary immunodeficiency due to defective nicotinamide adenine dinucleotide phosphate (NADPH) oxidase, resulting in failure of killing intracellular pathogens. Clinical presentation and management of these patients remains heterogeneous. Current management involves non-transplant therapy with interferon-gamma and supportive care, or hematopoietic stem cell transplant (HSCT) in severe cases. There has been limited data on morbidity and outcomes with different treatment options using patient registries. There has been no registry-based study of CGD patients from the United States comparing different treatment options.
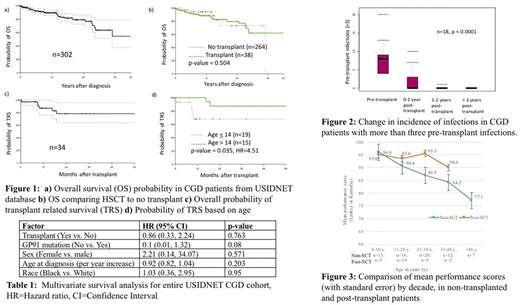
Methods: We performed a multi-institutional analysis of data from the United States Immunodeficiency Network (USIDNET) registry, comparing morbidity, mortality, and different treatment options. Retrospective review of data from its inception in 1992 through 2016 was performed. We analyzed demographic, co-morbidity and treatment information (HSCT versus non-transplant therapy). Logistic regression was used to compare overall survival (OS), transplant related survival (TRS) and frequency of serious infections and co-morbidities among the treatment groups. Multivariate logistic regression was used to evaluate factors affecting survival.
Results: Within the database, 507 CGD patients were identified, with 84% male. X-linked inheritance was most common (73%) with about 78% of patients having gp91 mutation. Of 507 patients, about 10% underwent HSCT (n=50). Overall mortality was 15% with relatively lower incidence in HSCT group (12%). In HSCT cohort, median age at transplant was 13.5 years (0.6-37.3 years), with 74% receiving reduced intensity conditioning (RIC). The most common graft source was peripheral blood stem cells (60%) from a matched-unrelated donor (72%). No mortality was reported in patients who received stem cells from matched siblings and in those who received bone marrow graft with RIC, at median follow-up of 24 months (range 3-402 months). Survival analysis included 302 patients. OS was not significantly different between HSCT and non-transplant groups (p=0.50; Figure 1 a, b). Among patients who underwent HSCT, there was significantly improved TRS in those transplanted before 14 years of age (p= 0.035, HR: 4.51; Figure 1 c, d). The proportion of patients who had >3 infections prior to transplant was significantly reduced by 2-years post-transplant (p < 0.0001, Figure 2). The rate of serious infections prior to transplant was significantly lower in patients transplanted at <14 years old compared to those transplanted at an older age (p< 0.001, 95% CI 19.2- 62.8). Stem cell source, graft type, conditioning regimen, and prior gamma-interferon treatment did not differ significantly between these two groups. Ten of 13 patients who had gastrointestinal granulomatous inflammation prior to transplant did not have documentation of disease at 1-35 months post-HSCT, with an additional subject experiencing relief of esophageal stricture post-transplant. In univariate analysis, patients with gp91 mutation had significantly worse survival compared to other mutations (p=0.008). In multivariate analysis for OS, gp91 mutation showed a trend towards significance within the entire cohort (p = 0.08, Table 1). Figure 3 shows comparison of mean quality of life (QoL) indicator for non-transplant (n=40) and post-transplant patients (n=12). The mean performance score was significantly higher in post-HSCT (93.33) patients compared to their non-transplant counterparts (84.73) for subjects 15 years or older (p=0.0021).
Conclusion: This is the largest reported American CGD cohort. HSCT at <14 years of age is associated with improved survival, decreased burden of serious infections, and granulomatous inflammation. Post transplant CGD patients have significantly better QoL as compared to non-transplant ones.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.